The 2025 World Lung Cancer Conference (WCLC) will be held by the International Association for the Study of Lung Cancer (IASLC) in Barcelona, Spain, from September 6th to 9th, 2025. As one of the most influential events in the global oncology community, WCLC provides a platform for academic exchange on the latest research findings and clinical experience for lung cancer experts and scholars worldwide. The conference announced key research indications primarily for non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). This article summarizes the hottest therapeutic targets and participating pharmaceutical companies presented at the conference.
1. EGFR
The epidermal growth factor receptor (EGFR), also known as HER1, is encoded by the ERBB1 gene and is a membrane-bound protein that belongs to the ERBB/HER receptor tyrosine kinase (RTK) family. This family also includes HER2 (ERBB2), HER3 (ERBB3), and HER4 (ERBB4). As the most prominent driver gene in NSCLC, EGFR is the subject of intense R&D competition, with a focus on addressing drug resistance. At this conference, several players presented clinical data on EGFR-targeted drugs, primarily focusing on third- and fourth-generation EGFR tyrosine kinase inhibitors (EGFR-TKIs).
- Osimertinib is a third-generation EGFR-TKI developed by AstraZeneca. At this conference, AstraZeneca released data from multiple combination studies involving 0simertinib, including osimertinib plus crizoxabin, osimertinib plus eltrobucin, and osimertinib plus savolitinib.
- Lazertinib is a third-generation EGFR-TKI developed by Johnson & Johnson. At the conference, Johnson & Johnson announced data from a study of lazertinib and amitriptyline combination therapy.
- Asandeutertinib (TY-9591) is an orally available, irreversible, third-generation EGFR inhibitor independently developed by TYK Medicines. It targets classic EGFR mutations (L858R or 19Del). A comparative study of its efficacy with osimertinib in patients with EGFR-mutated NSCLC and brain metastases was announced at the conference.
- HLX07, an innovative anti-EGFR monoclonal antibody developed by Henlius, specifically inhibits EGFR-related signaling pathways and enhances anti-tumor efficacy in combination with immunotherapy or chemotherapy. Updated data from a Phase II study of HLX07 combined with serotoninib (with or without chemotherapy) as a first-line treatment for squamous NSCLC with high EGFR expression were presented at the conference.
- Furmonertinib, a third-generation EGFR-TKI developed by Allist, exhibits broad activity and selectivity against EGFR mutations. Updated data from the PACC cohort of the Phase 2 FURTHER trial (FURMO-002; NCT05364073) were presented at the meeting. Vometinib, which has high central nervous system (CNS) penetration, demonstrated antitumor activity in a range of patients with NSCLC harboring EGFR PACC mutations.
2. MET
Mesenchymal epithelial transition factor (MET), also known as c-MET, is a receptor tyrosine kinase. Normally, the MET protein is involved in cell growth and repair. However, in lung cancer patients, abnormalities in the MET gene can lead to continued cancer cell growth, metastasis, and drug resistance. METex14 skipping mutations and MET amplification are important mechanisms of drug resistance and primary driver genes in lung cancer. The main players presenting updated data at this conference were Merck and Novartis.
- Tepotinib, the world’s first approved MET inhibitor, was developed by Merck. It is an oral, highly selective MET tyrosine kinase inhibitor designed to inhibit the oncogenic signaling pathway driven by MET gene mutations. Data from the VISION study (≥3 years of follow-up analysis) were presented at this conference, demonstrating a favorable long-term safety profile for tepotinib.
- Capmatinib, developed by Novartis, is a highly bioavailable and selective oral MET receptor tyrosine kinase inhibitor. Since May 2020, capmatinib has been approved for marketing in multiple countries and regions, including the United States, Japan, the European Union, and Switzerland. It is recommended as a priority treatment for the full range of NSCLC patients with MET exon skipping in international lung cancer guidelines. The first real-world study of capmatinib in China for the treatment of MET amplification was announced at this conference, providing important evidence for the clinical application of this targeted drug in the Chinese population.
3. KRAS
The Kirsten murine sarcoma viral oncogene (KRAS) is a gene located on human chromosome 12 that encodes the KRAS protein. This protein belongs to the small GTPase family and dynamically switches between an active GTP-bound state (KRAS(ON)) and an inactive GDP-bound state, regulating cell proliferation, survival, and other signaling pathways. Once considered an “undruggable” target, KRAS has now become a hot topic of competition, particularly the G12C mutation. This mutation is common among KRAS mutations and is often found in pancreatic ductal adenocarcinoma, colorectal cancer, and lung adenocarcinoma (especially in patients with no history of smoking and inadequate response to PD-1 inhibitors alone). At the conference, players such as Amgen and Bristol-Myers Squibb updated their pipeline research data.
- Sotorasib, also known as Lumakras, is an oral KRAS G12C inhibitor developed by Amgen. It covalently binds to the switch pocket of the KRAS G12C mutant protein, specifically inhibiting GTPase activity and blocking the aberrant activation of the RAS signaling pathway. This drug received accelerated approval from the US FDA on May 28, 2021, for the treatment of patients with locally advanced or metastatic NSCLC harboring the KRAS G12C mutation. The meeting announced primary endpoint results from the Phase II SHERLOCK trial, a combination of sotorasib, bevacizumab, and chemotherapy in patients with advanced NSCLC harboring the KRAS G12C mutation.
- GFH375 is an oral, highly active, and highly selective small molecule KRAS G12D (ON/OFF) inhibitor independently developed by GenFleet Therapeutics. Data from its Phase I/II clinical study for the treatment of KRAS G12D-mutant solid tumors, particularly NSCLC, were presented at the meeting.
- Olomorasib (LY3537982) is a potent and highly selective second-generation KRAS G12C inhibitor under development by Eli Lilly. The 2025 World Cancer Liver Cancer Conference (WCLC) presented integrated analysis data from its combination with chemotherapy and immunotherapy for the treatment of advanced KRAS G12C-mutant NSCLC.
- Adagrasib (Krazati) is an irreversible inhibitor targeting the KRAS G12C mutation, developed by Mirati Therapeutics, a US biopharmaceutical company. It was approved for marketing in late 2022 for the treatment of KRAS G12C-mutant NSCLC (patients who have received at least one prior systemic therapy). Results from a Phase 3 clinical study of adagrasib in combination with pembrolizumab and chemotherapy in patients with advanced KRAS G12C-mutant NSCLC were presented at the 2025 WCLC conference.
- Fulzerasib (GFH925, IBI351) is an irreversible inhibitor targeting the KRAS G12C mutation, developed by Innovent Biologics. The meeting announced results on the effects of cetuximab combined with either sotorasib or fulzerasib on fumaric acid and Ass1 in KRAS-mutant NSCLC patients.
In addition, other domestic pharmaceutical companies developing KRAS G12C inhibitors include Jacobio Pharmaceuticals and Innovent Biologics. JAB-21822, developed by Jacobio Pharmaceuticals, was approved for marketing in May 2025.
4. RET
Rearranged during transfection (RET) is a receptor tyrosine kinase gene and a proto-oncogene that everyone carries. Under normal circumstances, the RET gene is regulated by the body itself and does not cause excessive growth of normal or tumor cells. However, abnormal changes in the RET gene can lead to the development of cancer cells. Tumor-associated RET gene abnormalities include gene mutations and gene fusions. RET fusions are the most common RET gene abnormality associated with NSCLC. Although they only account for 1%–2% of all non-small cell lung cancers, due to the large lung cancer patient population, affected patients are not uncommon. Updated clinical data for multiple drugs were released at the 2025 WCLC.
- Selpercatinib is a potent, highly selective oral RET tyrosine kinase inhibitor developed by Loxo Oncology, whose pipeline was acquired by Eli Lilly for $8 billion in 2019. Selpercatinib received its first approval from the US FDA in May 2020, becoming the world’s first approved highly selective RET inhibitor. Results from a multicenter retrospective study of FHND5071 for the treatment of advanced or recurrent RET fusion-positive NSCLC in Japan were presented at the 2025 WCLC.
- FHND5071, a next-generation RET inhibitor independently developed by Zhengda Fenghai, is a broad-spectrum and highly selective inhibitor primarily for the treatment of RET fusion-positive and mutation-positive advanced solid tumors. Results from a Phase I clinical trial in patients with RET fusion-positive advanced NSCLC were also presented at the conference.
- Pralsetinib, a potent and highly selective RET inhibitor developed by Blueprint Medicines, inhibits phosphorylation of RET and its downstream molecules, effectively suppressing the proliferation of cells expressing RET gene mutations. The drug was first launched in the US in May 2020. Final data from the Phase 1/2 ARROW study were presented at the conference, demonstrating its efficacy and safety in patients with advanced RET fusion-positive NSCLC.
5. ROS1
The c-ros oncogene 1 (ROS1) belongs to the insulin receptor family of receptor tyrosine kinase genes. Under normal circumstances, the ROS1 protein it encodes participates in signaling pathways that regulate cell growth and proliferation. In the field of precision medicine diagnosis and treatment of NSCLC, ROS1 fusions are relatively rare driver gene mutations, occurring in approximately 1%-3%, making them rare targets.
- Taletrectinib is a next-generation ROS1 tyrosine kinase inhibitor (TKI) developed by Daiichi Sankyo. In December 2018, development, manufacturing, and commercialization rights were granted to AnHeart Therapeutics. In June 2021, Innovent Biologics and AnHeart Therapeutics entered into a collaboration agreement to jointly develop and commercialize taletrectinib in Greater China and jointly promote its application in the region. Subsequently, in April 2024, AnHeart Therapeutics was acquired by Nuvation Bio, further accelerating the development and commercialization of taletrectinib. The meeting announced the results of multiple clinical studies of Taletrectinib, including the Phase 2 TRUST-I study, TRUST-II study, and TRUST-III study.
6. HER2
Human epidermal growth factor receptor 2 (HER2) is a transmembrane tyrosine kinase receptor on the cell surface, belonging to the epidermal growth factor receptor (EGFR) family. Abnormal HER2 signaling is associated with various cancers, particularly breast and gastric cancers. In NSCLC, HER2 mutations (not amplifications) have become a clear therapeutic target, with antibody-drug conjugates (ADCs) currently the mainstream approach.
- Trastuzumab Deruxtecan is an anti-HER2 ADC jointly developed by AstraZeneca and Daiichi Sankyo. It combines a HER2-targeting antibody with a highly potent cytotoxic drug, enabling direct delivery of the toxin to tumor cells. It has demonstrated significant efficacy in multiple clinical trials. Data from several clinical studies, including DESTINY-Lung06 and DESTINY-Lung05, were presented at the meeting. DESTINY-Lung06 highlighted the efficacy and safety of trastuzumab deruxtecan plus pembrolizumab combination therapy as a first-line treatment for patients with HER2+ NSCLC and PD-L1 Tps <50%. DESTINY-Lung05 highlighted the final results of trastuzumab deruxtecan in Chinese patients with HER2-mutant NSCLC.
- TQB2102, a HER2-positive bispecific antibody-ADC developed by CHIA TAI TIANQING PHARMACEUTICAL GROUP, utilizes a dual-epitope design (binding to ECD2 and ECD4 on the surface of HER2-positive tumor cells) to enhance targeted killing of HER2-abnormal tumors, avoiding the limitations of traditional monoclonal antibodies or single-target ADCs. This drug is the first HER2-positive bispecific antibody-ADC to enter clinical trials for the treatment of NSCLC caused by HER2 abnormalities. Phase II clinical data from this study will be released at the 2025 WCLC for patients with locally advanced/metastatic HER2-abnormal NSCLC who have failed at least one prior line of therapy.
In addition, other pharmaceutical companies targeting the HER2 target in lung cancer include Bliss Biopharmaceutical (BB-1701, EGFR/HER2 ADC) and Kelun Biotech (A166, HER2 ADC).
7. PD-L1
Programmed death ligand 1 (PD-L1), a classic immune checkpoint, has seen intense competition in immunotherapy. Currently, the focus of PD-L1 immunotherapy is on novel combination therapies and novel immunotherapies. At this conference, bispecific/combination therapies were a hot topic in PD-L1-related therapies, and data exploring PD-L1 as an ADC target were also presented.
- Anti-PD-L1 combination therapies are exemplified by tarlatamab plus anti-PD-L1. Tarlatamab, a bispecific T cell-engaging immunotherapy developed by Amgen that targets delta-like ligand 3 (DLL3), has been shown to improve survival in previously treated small cell lung cancer (SCLC). Data from the Phase I DeLLphi-303 study were presented at WCLC 2025. This study evaluated the safety and efficacy of tarlatamab combined with either atezolizumab or durvalumab as first-line maintenance therapy for patients with extensive-stage (ES) SCLC. Pumitamig is a PD-L1 x VEGF-A bispecific antibody jointly developed by BioNTech and Bristol-Myers Squibb. Data from a Phase I/II study in early-line SCLC were presented at this conference. The data showed that Pumitamig plus chemotherapy demonstrated acceptable efficacy and safety in first-line or early-line SCLC, with strong anti-tumor activity.
- HLX43 is an innovative PD-L1 antibody-drug conjugate (ADC) developed by Henlius. This drug targets PD-L1 and precisely delivers its payload via an ADC to exert its anti-tumor effects. A Phase I clinical study evaluating the safety, tolerability, and preliminary efficacy of HLX43 in advanced/metastatic solid tumors was presented at this conference. The abstract stated: “Early studies of HLX43 in advanced/metastatic solid tumors demonstrated a manageable safety profile and preliminary efficacy signals.”
8. NTRK
The NTRK family consists of three members, NTRK1, NTRK2 and NTRK3, encoding TRK family proteins, TRKA, TRKB, and TRKC, respectively. TRKs are activated in malignant tumors through a variety of mechanisms, including NTRK gene fusions, TRK protein overexpression, or single nucleotide alterations. TRKs are rare in lung cancer but have high efficacy. This meeting did not present a large amount of new, validated data for first-in-class NTRK therapies, but rather focused on long-term follow-up/longitudinal data, evidence of activity in the brain, and updates and discussions on resistance and research directions for second-generation inhibitors.
- Larotrectinib is a first-generation, highly selective NTRK/TRK inhibitor developed by Bayer. Presentations at the meeting highlighted the long-term tolerability and durable responses of larotrectinib in TRK fusion-positive solid tumors, including efficacy data and real-world comparative analyses in patients with central nervous system (CNS) tumors and brain metastases. Long-term data support its strong position in NTRK fusion cancers.
- Entrectinib is a TRK/ROS1 inhibitor with activity against brain metastases, developed by Roche. WCLC report highlights entrectinib’s intracranial responses in NTRK fusion tumors and activity against CNS metastases.
9. Emerging Targets
In addition to the targets mentioned above, several emerging targets, such as B7-H3、TROP2、FRa and DLL3, emerged at the 2025 WCLC meeting. These targets are often developed through bispecific antibodies or ADCs and represent future growth areas.
TROP2-targeted therapies are exemplified by Gilead’s sacituzumab govitecan, a TROP2 ADC. Its Phase III clinical study in patients with extensive-stage small cell lung cancer was presented at the meeting.
B7-H3-targeted therapies are exemplified by Qilu Pharmaceutical’s QLC5508, a B7-H3 ADC. Its payload is the topoisomerase inhibitor SuperTopoi™, which is 5-10 times more potent than DXd. Updated data from its Phase I study in previously treated extensive-stage SCLC patients were presented at the 2025 WCLC meeting.
DLL3-targeted therapies are exemplified by Hengrui Medicine’s independently developed Category 1 novel drug SHR-4849, a DLL3 ADC with a topoisomerase inhibitor (TOPOi) as its payload. At the 2025 WCLC meeting, Hengrui reported for the first time the results of a Phase I clinical study of SHR-4849 in patients with relapsed SCLC. This study was a multicenter, open-label Phase I clinical trial consisting of dose escalation and dose expansion phases.
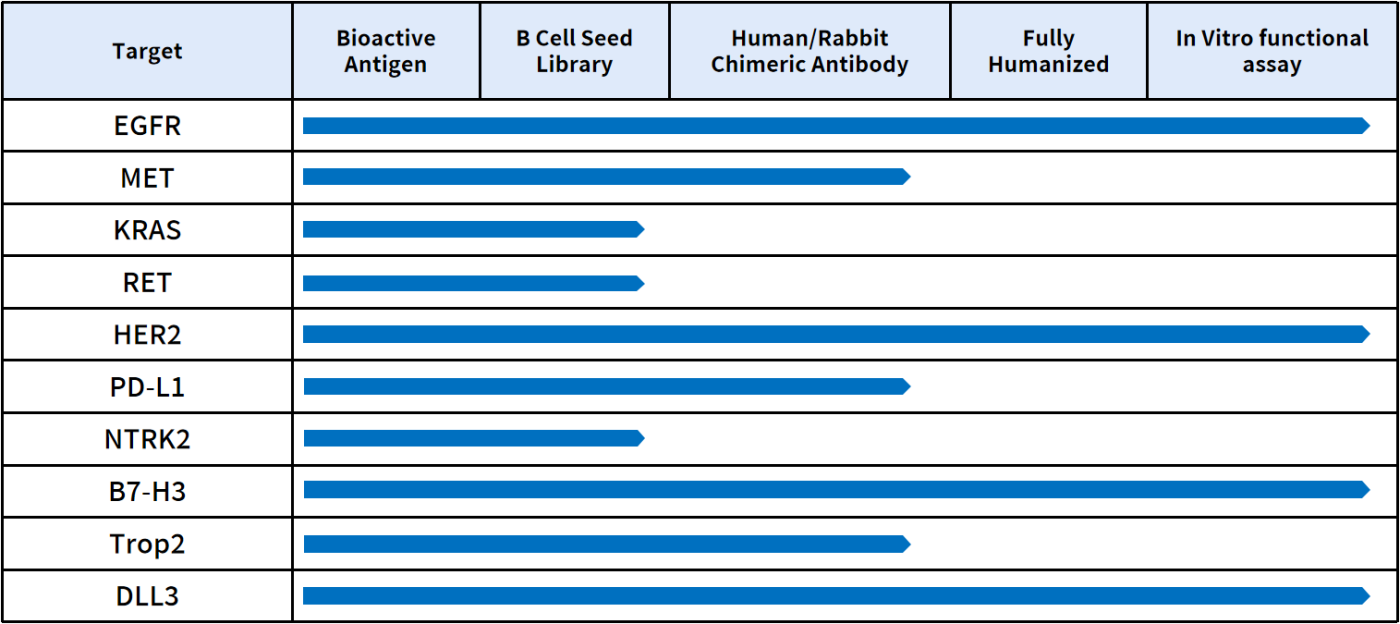
10. 5,000+ IgG Sequences Ready to Licensing-out
DMAB BIOTECH is a biotechnology company focused on providing products and services to biopharmaceutical companies. Unlike traditional CROs, we offer functionally validated, off-the-shelf lead antibody molecules. We have developed over 5,000 off-the-shelf lead antibody molecules targeting over 500 popular drug targets, with confirmed antibody sequences and validation data. We have also applied for patents on all existing sequences, with global licensing available. You can instantly import data packages for molecular testing without waiting. We have also established a comprehensive preclinical pharmacodynamic evaluation platform for ADC antibody discovery.
For more details on lead molecules, please call email us at info@dimabio.com / orders@dimabio.com.

